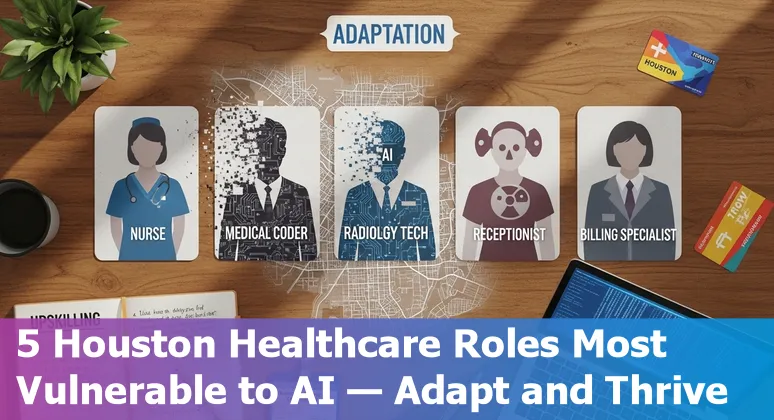
Top 5 Jobs in Healthcare That Are Most at Risk from AI in Houston - And How to Adapt
Last Updated: August 19th 2025
Too Long; Didn't Read:
Houston healthcare roles most at risk from AI: radiologic technologists, pathologists/techs, medical coders, triage nurses, and scribes. AI pilots cut report time up to 40%, RCM costs ~70%, trim A/R days (75→55), and save ~57 nurse hours/1,000 calls - reskill into AI oversight, QA, and analytics.
Houston healthcare workers should care about AI because it's rapidly shifting from pilot projects to everyday clinical infrastructure - AI tools are already helping spot fractures, prioritize ambulance transfers and cut documentation time, which directly affects hospital throughput and clinician workload (see the World Economic Forum guide to AI in healthcare: https://www.weforum.org/stories/2025/08/ai-transforming-global-health/).
Practical pilots in Houston, like targeted post-discharge monitoring strategies in Houston that lower 30‑day readmissions, already lower 30‑day readmissions, so learning to operate and evaluate AI is a defensible career move; Nucamp's Nucamp AI Essentials for Work 15-week bootcamp teaches those workplace AI skills in 15 weeks for clinicians who want to adapt rather than be disrupted.
| Bootcamp | Key details |
|---|---|
| AI Essentials for Work | 15 weeks • Practical AI tools & prompt-writing • Early bird $3,582 • Register for Nucamp AI Essentials for Work (15-week bootcamp) |
“…it's essential for doctors to know both the initial onset time, as well as whether a stroke could be reversed.” - Dr Paul Bentley
Table of Contents
- Methodology: How we identified the top 5 at-risk healthcare jobs for Houston
- 1. Radiologic Technologists (X-ray, CT, MRI) - Risk and adaptation
- 2. Pathologists / Pathology Lab Technicians - Risk and adaptation
- 3. Medical Coders and Billing Specialists - Risk and adaptation
- 4. Primary Care Triage Nurses / Nurse Triage Call Centers - Risk and adaptation
- 5. Medical Transcriptionists and Clinical Scribes - Risk and adaptation
- Conclusion: Next steps for Houston healthcare workers and resources in Texas
- Frequently Asked Questions
Get actionable advice on protecting patient privacy under Texas rules when deploying AI tools.
Methodology: How we identified the top 5 at-risk healthcare jobs for Houston
(Up)This analysis prioritized Houston-relevant evidence and three objective criteria: degree of routineness, measurable automation impact, and local adoption. Sources included industry forecasts showing rapid task automation - Healthcare IT Today projects AI agents handling 50–60% of front‑office work and RCM cost reductions up to 70% in 2025 - so roles dominated by documentation, billing, or rule‑based image review scored high for risk (Healthcare IT Today 2025 AI predictions for healthcare front-office automation).
Workforce strain and hard ROI made another cut: nearly half of hospitals report staffing gaps and administrative spending drives major waste, making automation readiness essential per recent workflow analysis (CSI 2025 workflow automation analysis for healthcare efficiency).
Finally, local pilots and case studies in Houston - such as targeted post‑discharge monitoring that already lowers 30‑day readmissions - confirmed real-world feasibility and helped weight roles by local impact and transition pathways (Houston post-discharge AI case studies reducing 30-day readmissions).
The result: jobs with high repetitive administrative load, heavy documentation, or standardized image/text review rose to the top as most at risk and most in need of reskilling.
1. Radiologic Technologists (X-ray, CT, MRI) - Risk and adaptation
(Up)Radiologic technologists in Houston face near-term task automation across ordering, protocol selection, patient positioning, dose optimization, image post‑processing and even draft reporting - areas identified by Hardy et al., Br J Radiology study on AI-driven workflow change in diagnostic imaging and by industry guidance that flags protocoling and image‑acquisition as high‑yield automation points in The Doctors Company article on using AI to improve radiology workflow.
Clinical pilots now show these tools can materially speed throughput - one system reported average report efficiency gains of 15.5% and site-level gains up to 40% - which means routine review and gating tasks traditionally done by techs will increasingly be delegated to AI unless technologists expand into oversight, AI auditing, cross‑modality competencies and stronger patient‑facing roles to retain value, as reported in a Northwestern Medicine study on AI transforming radiology with speed and accuracy.
The concrete so‑what: mastering AI basics and QA workflows (protocol validation, dose checks, and documenting when an algorithm is overridden) converts rapid automation risk into new clinical leadership opportunities for Houston rad‑techs.
“This is, to my knowledge, the first use of AI that demonstrably improves productivity, especially in health care… I haven't seen anything close to a 40% boost.” - Dr. Mozziyar Etemadi
2. Pathologists / Pathology Lab Technicians - Risk and adaptation
(Up)Pathologists and pathology lab technicians in Houston face rapid task-level automation as whole-slide imaging and AI move from research to routine use - systems that pre-screen slides, score PD‑L1, and flag suspicious regions are already cutting courier delays, enabling remote reads and reshaping daily workflows (Sagis digital pathology and AI transformation).
Local adoption shows real-world impact: UTMB now creates AI-generated overlays on every prostate biopsy to highlight areas human reviewers can miss, shortening turnaround and creating new consult pipelines for the health system (UTMB AI-enabled prostate biopsy overlays clinical adoption).
At the same time, peer-reviewed work demonstrates AI's clinical promise to provide quantitative, objective support in what has long been a subjective discipline - opening opportunities for pathologists who can validate models, manage WSI QA, and lead multidisciplinary AI governance (Journal of Medical Imaging review of AI in digital pathology).
The so‑what: technicians who learn slide scanning, WSI troubleshooting, and algorithm auditing can convert automation risk into higher-value roles (remote consult coordination, AI oversight, and biomarker annotation) while helping Houston labs reduce turnaround time and attract specialty referrals.
“Prostate cancer is legendary as being difficult to diagnose… Not because it is rare but because the cancer mimics normal tissue, so it becomes incredibly difficult for pathologists to make sure they are not missing that little malignant gland of prostate cancer lurking among the many benign glands that are always present in the prostate.” - Dr. Harsh Thaker
3. Medical Coders and Billing Specialists - Risk and adaptation
(Up)Medical coders and billing specialists in Houston sit squarely in the crosshairs of RPA and AI: bots now perform eligibility checks, claims submission, payment posting, and even first‑pass coding reviews, cutting errors and accelerating reimbursement while integrating with legacy EHRs (RPA benefits for medical billing and revenue cycle management).
The practical consequence is stark - real-world programs have cut billing costs dramatically and trimmed A/R days (one case reduced A/R from 75 to 55 days, freeing roughly $14M in working capital), so billing teams that only handle repetitive entry risk shrinking headcount as payers and vendors scale automation (RPA automation replacing manual medical billing processes).
The adaptation strategy is clear and tangible: pivot from line‑item entry to exception management, denial prevention, AI‑audit governance, and analytics-driven revenue recovery - skills that preserve value by resolving the 10–20% of claims bots can't reliably adjudicate.
For Houston practices and RCM shops, mastering RPA oversight and advanced coding/appeal workflows turns an automation threat into a faster, higher‑margin service offering.
4. Primary Care Triage Nurses / Nurse Triage Call Centers - Risk and adaptation
(Up)Primary‑care triage nurses and Houston nurse‑triage call centers face quick task automation as virtual triage and chatbots take on symptom collection, urgency scoring and scheduling; studies show AI can handle a large share of routine queries - reducing average triage time to about five minutes and saving roughly 57 nurse work hours per 1,000 calls - so the immediate risk is headcount loss on repeat assessments but the clear adaptation path is to become the human‑in‑the‑loop: validate algorithm outputs, manage exceptions, audit bias, and own escalation protocols.
Local clinics and payers that deploy Infermedica‑style virtual triage report meaningful diversion of low‑acuity visits and faster routing of serious cases, while nursing reviews highlight AI's role in lowering documentation burden and cognitive load when designed for nurse–AI collaboration; multilingual, EHR‑integrated implementations common in U.S. settings make these tools practical for Houston's diverse patient panels.
The practical “so what?”: nurses who add triage‑AI governance, clinical decision‑support oversight, and EHR integration skills convert automation risk into leadership roles that preserve clinical judgment and improve throughput (Infermedica virtual triage study on nurse call center efficiency, systematic review of AI in nursing (PMC), analysis of AI chatbots handling routine triage queries).
| Metric | Impact |
|---|---|
| Routine queries handled | Up to 80% (AI chatbots) |
| Average triage call time | ~5 minutes (virtual triage) |
| Nurse hours saved | 57 hours per 1,000 calls |
| Estimated savings | $175 per interview (U.S. estimate) |
"We needed a CDSS that could tolerate and analyze multiple symptoms, reflect real consultation with risk factors... provide a more comprehensive and accurate triage." - Dr. Nirvana Luckraj
5. Medical Transcriptionists and Clinical Scribes - Risk and adaptation
(Up)Medical transcriptionists and clinical scribes in Houston face immediate task compression as Automatic Speech Recognition (ASR) and ambient‑AI scribes turn spoken visits into structured EHR notes in minutes, not days - AI systems can transcribe a 30‑minute recording in about five minutes versus human turnaround measured in days - so the routine typing and first‑pass note work that has sustained these roles is shrinking.
When implemented well, AI cuts charting time, reduces denials with more complete notes, and reclaims provider hours (Commure pilots report clinicians saving 5+ minutes per visit and some reclaiming hours each day), but accuracy still hinges on specialty lexicons, accents, audio quality and HIPAA‑safe pipelines, meaning human review remains essential (Commure analysis of AI medical transcription clinical and financial impact, Simbo.ai analysis of AI and speech recognition impact on medical transcription services).
The clear adaptation path for Houston transcriptionists and scribes: shift into human‑in‑the‑loop roles - editorial QA, specialty lexicon training, EHR‑integration specialists and AI‑safety auditors - so that faster notes translate into safer, billable, and reimbursable records rather than lost jobs.
“I know everything I'm doing is getting captured and I just kind of have to put that little bow on it and I'm done.”
Conclusion: Next steps for Houston healthcare workers and resources in Texas
(Up)Houston clinicians should treat AI like a new medical device: read the practical JAMA safety recommendations from UTHealth/Baylor, stand up local governance, and build routine testing and clinician training into deployments so AI augments - not replaces - clinical judgment; the JAMA guidance lists concrete steps (multidisciplinary committees, inventories, turn‑off procedures and clinician training) that Houston health systems can adopt now (UTHealth/Baylor JAMA guidance for AI safety in clinical care).
Pair that operational approach with legal and compliance planning - Morgan Lewis lays out why robust AI governance, written policies, monitoring, and transparency matter to avoid enforcement and False Claims Act risk (including recent Texas enforcement examples) (Morgan Lewis AI compliance primer for healthcare) - and explicitly audit datasets for representation gaps (women and low‑income or minority patients are underrepresented in training data per recent PubMed analysis), because equity failures create safety and legal exposure (AI and health equity study on PubMed).
For individual workers: practical reskilling (AI oversight, prompt‑writing, QA and analytics) is the fastest path to retain value - Nucamp's 15‑week AI Essentials for Work bootcamp teaches workplace AI skills, prompt design and real‑world governance basics and is a clear, short pathway for Houston staff to move into human‑in‑the‑loop roles (Nucamp AI Essentials for Work bootcamp - 15 weeks, early bird $3,582).
| Resource | Why it helps |
|---|---|
| UTHealth/Baylor JAMA guidance for AI safety in clinical care | Concrete clinical governance and testing checklist for safe AI use |
| Morgan Lewis AI compliance primer for healthcare | Regulatory and enforcement risks, compliance program elements |
| Nucamp AI Essentials for Work bootcamp - 15 weeks | Practical AI skills for clinicians: prompts, governance, workplace use |
“Health care delivery organizations will need to implement robust governance systems and testing processes locally to ensure safe AI and safe use of AI so that ultimately AI can be used to improve the safety of health care and patient outcomes.” - Hardeep Singh, MD, MPH
Frequently Asked Questions
(Up)Which five healthcare jobs in Houston are most at risk from AI and why?
The analysis identifies Radiologic Technologists, Pathologists/Pathology Lab Technicians, Medical Coders and Billing Specialists, Primary Care Triage Nurses (including nurse‑triage call centers), and Medical Transcriptionists/Clinical Scribes as most at risk. Each role scores high on routineness, measurable automation impact, and local adoption: imaging protocoling and post‑processing for rad‑techs; whole‑slide imaging pre‑screening for pathology; RPA and AI for coding and claims; virtual triage/chatbots for triage nursing; and ASR/ambient‑AI for transcription and scribe work. Local pilots and industry forecasts show these tasks are already being automated or augmented, reducing headcount for routine tasks unless workers reskill into oversight and higher‑value functions.
What concrete adaptation strategies can Houston healthcare workers use to stay valuable?
Across roles the practical adaptation is to move from routine task execution to human‑in‑the‑loop responsibilities: learn AI basics, QA and algorithm auditing, prompt writing, EHR/WSI integration and troubleshooting, exception management, denial prevention and analytics, clinical governance and bias auditing, and patient‑facing or multidisciplinary leadership tasks. Examples: radiologic technologists should master protocol validation and AI QA; path techs should learn slide scanning, WSI troubleshooting and model validation; coders should pivot to exception workflows and RPA oversight; triage nurses should own escalation protocols and AI audit; scribes should specialize in editorial QA and specialty lexicons.
How urgent is reskilling and what training options are practical for clinicians in Houston?
Reskilling is urgent because AI is moving from pilots to operational infrastructure - tools are already improving throughput (example: 15.5% avg. report efficiency gains, site gains up to 40%) and reducing administrative costs. Short, targeted programs that teach workplace AI skills, prompt design, governance and QA are practical. Nucamp's AI Essentials for Work is one example: a 15‑week bootcamp focused on practical AI tools and prompt writing aimed at clinicians seeking human‑in‑the‑loop roles. Complement training with local governance familiarity (JAMA safety recommendations) and compliance/legal basics.
What local Houston evidence supports these risk rankings and potential ROI from automation?
The methodology weighted local adoption and pilots: Houston programs using targeted post‑discharge monitoring have already lowered 30‑day readmissions; UTMB uses AI overlays on prostate biopsies to shorten turnaround; site pilots reported up to 40% productivity boosts in imaging; RCM programs have cut A/R days (example: from 75 to 55 days freeing ≈$14M). Additionally, studies of virtual triage show reductions in triage time (~5 minutes) and savings (≈57 nurse hours per 1,000 calls). These local and sector examples demonstrate real ROI and real displacement risk for routine tasks.
What governance, safety and equity steps should Houston health systems and workers prioritize when adopting AI?
Treat AI like a medical device: implement multidisciplinary AI governance committees, maintain inventories of deployed models, define turn‑off procedures, require clinician training and routine testing (per JAMA guidance). Address compliance and legal exposure by documenting governance and monitoring (per regulatory guidance), audit datasets for representation gaps (women, low‑income and minority underrepresentation), and build transparency and bias mitigation into deployments. Workers should gain skills in AI auditing, dataset review, and safety testing to support these system‑level safeguards.
See why post-discharge monitoring strategies in Houston are lowering 30-day readmission rates after targeted follow-ups.
Learn how multimodal genomics and imaging with AIGI is enabling new biomarker discovery at UTHealth Houston.
Ludo Fourrage
Founder and CEO
Ludovic (Ludo) Fourrage is an education industry veteran, named in 2017 as a Learning Technology Leader by Training Magazine. Before founding Nucamp, Ludo spent 18 years at Microsoft where he led innovation in the learning space. As the Senior Director of Digital Learning at this same company, Ludo led the development of the first of its kind 'YouTube for the Enterprise'. More recently, he delivered one of the most successful Corporate MOOC programs in partnership with top business schools and consulting organizations, i.e. INSEAD, Wharton, London Business School, and Accenture, to name a few. With the belief that the right education for everyone is an achievable goal, Ludo leads the nucamp team in the quest to make quality education accessible


